Precision medicine
Giving the right medicine, to the right patient, at the right time
What is precision medicine?The EFPIA Precision Medicine Working Group has developed the following definition of Precision Medicine:
“Precision medicine is a healthcare approach that utilises molecular information (genomic, transcriptomic, proteomic, metabolomic, etc), phenotypic and health data from patients to generate care insights to prevent or treat human disease resulting in improved health outcomes”.
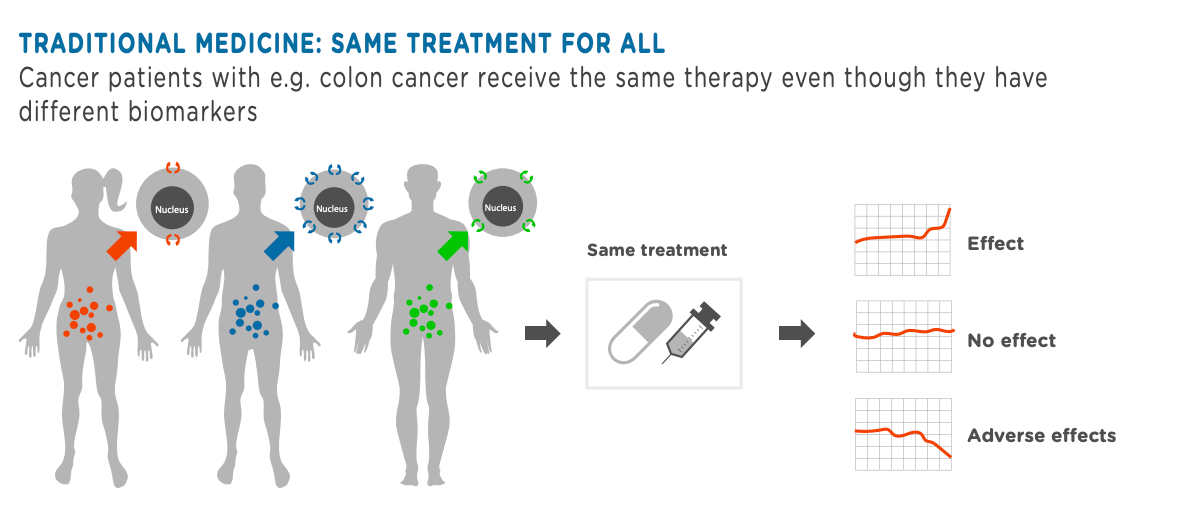
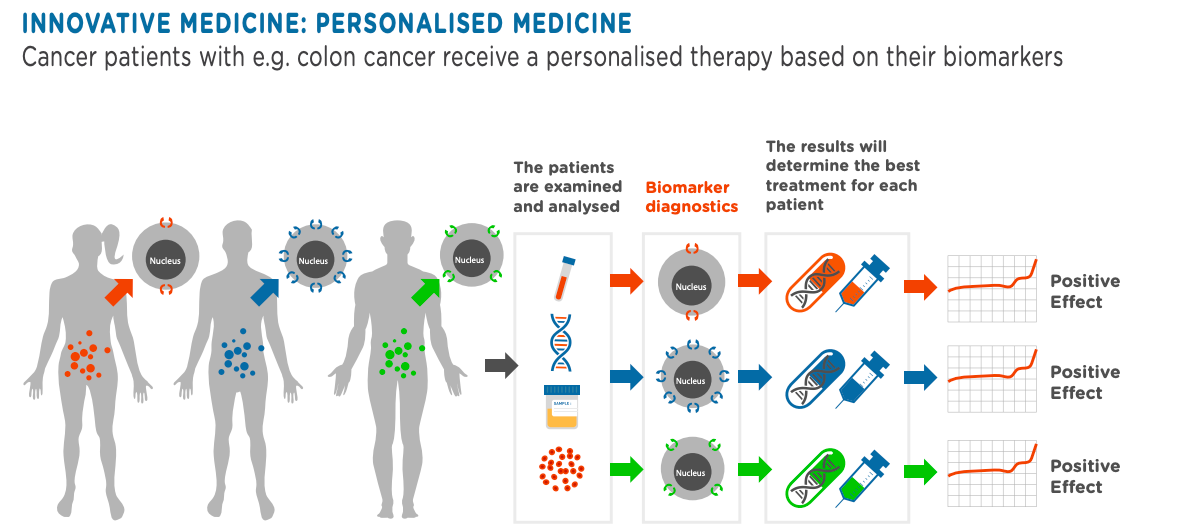
Precision medicine is based on an increased understanding of the molecular mechanism of diseases, so we are now better able to group patients who would best benefit from a specific treatment. It addresses the common observation that patients with apparently the same clinical diagnosis or symptoms often exhibit different responses to the same treatment.
Precision medicine targets treatments to patients who are most likely to benefit from them, in contrast to the traditional “one size fits all” approach to prevention and care.
The ability to target therapies relies on patient characteristics called biomarkers[1], which are indicators of pathological processes or markers of response to a treatment. These are objectively measured biological traits, which can be of many different types e.g. genetic, levels of substances in blood, imaging. A patient’s biomarker status is determined with the aid of modern diagnostic tools, in particular with so-called companion diagnostic tests or next generation sequencing[2]. These are used to identify patients who will either benefit from a specific medicine, or who may be at risk of particularly severe side effects.
How does biomarker testing work?Ever increasing knowledge of biomarkers is driving the use of broader tests, allowing for precise treatment decisions and monitoring. Biomarker testing exists in a complex health ecosystem – with physicians, patients, hospitals, laboratories, pharmaceutical companies, universities, patient organisations, public-private partnerships, governments, regulators, health technology assessment bodies, among others – all playing a crucial role in enabling access to biomarker testing and unlocking the potential of precision medicine.

Why is precision medicine so important ?
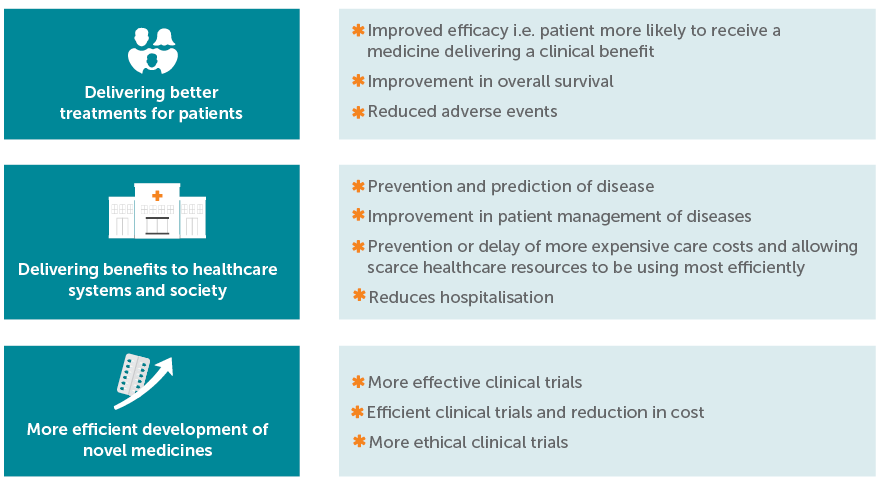
Giving the right treatment to the right person at the right time is leading to better outcomes for patients. It is also expected to reduce risk of adverse effects for patients at the same time as reducing costs and improving the sustainability and efficiency of healthcare systems.
What are the benefits of precision medicine?
The benefits of PM can be classified into three main categories:
1 A biomarker is a biological characteristic that is objectively measured and evaluated as an indicator of biological processes. “Biomarker” refers to any molecule in the human body that can be measured to assess health. Molecules can be derived from blood, body fluids or tissue. A biomarker test is a biochemical measurement developed to quantitate one, or several, biomarkers for the screening, diagnosis and/or prognosis of cancer patients for example.
2 Next generation sequencing (NGS): large-scale DNA sequencing technology in which millions of nucleotide sequences are deciphered simultaneously. Allows for querying the entire genome (whole genome), the exons within all known genes (whole exome) or only exons for selected genes (target panel)
Related resources
- Adoption Of Precision Health And Precision Medicine Approaches In Addressing Population Health Needs In Europe get_app
- Call to action to the European Commission to postpone and facilitate a phased implementation of the in vitro diagnostic Regulation get_app
- Unlocking the potential of precision medicine in Europe: Improving cancer care through broader access to quality biomarker testing get_app
- Infographic: Unlocking the potential of precision medicine in Europe – improving cancer care through broader access to quality biomarker testing summary.pdf get_app
- Access to Personalised Oncology in Europe get_app
- Determining the Path for Assessment of a Companion Diagnostic (CDx) under the In Vitro Diagnostic Medical Devices Regulation get_app
- The benefits of personalised medicine to patients, society and healthcare systems get_app
- EFPIA EBE personalised medicine manifesto 2017 get_app
- EBE White Paper on Personalised Medicine get_app