Transforming the lives of people living with cardiovascular diseases
The way forward to tackle Europe’s #1 killer
Our Vision is to reduce premature mortality and disabilities from Cardiovascular Diseases, Europe’s #1 killer. We seek to do this by prioritizing the importance of early intervention and secondary prevention as well as fostering innovation to transform cardiovascular health and improve outcomes for patients.
Sixty million people are living with cardiovascular diseases (CVDs) in the EU, and 13 million new cases of CVD are diagnosed every year. Every day 5,000 Europeans lose their lives due to CVD like heart attacks or strokes. And the pandemic has made it worse: the millions of people with undetected CVDs were 5 times more likely to die. Each of those deaths is a loss to a family, to a community and to society and the most shocking part of this situation is that the majority of deaths would have been avoidable through effective public health and prevention interventions or through timely and effective health care interventions.
Our mission: Improve CVD patients’ lives
The EFPIA Cardiovascular Health Platform represents ten EFPIA member companies committed to R&D in cardiovascular disease, an area with still high unmet need, with the aim to highlight the importance of early detection, the right diagnosis, and secondary prevention for improving CVD patients’ lives in Europe.
The Platform strives to achieve this by emphasizing the cost effectiveness of investing in cardiovascular health, CVD prevention and screening, to improve health outcomes and reduce the disease burden and the resulting disabilities at population level, thereby improving the sustainability and resilience of healthcare systems and of the economy overall.
A focus area of the EFPIA Cardiovascular Health Platform is building the evidence to drive better policy proposals and innovative solutions, supporting CVD-patients, their caregivers as well as health-care professionals. Close collaboration with all relevant stakeholders in the CVD-field is needed to successfully achieve this. In this regard, EFPIA actively supports the European Alliance of Cardiovascular Health (EACH) to boost policy action and awareness together with 16 other partner organizations in the CVH space. EACH is an active consortium that recognizes the need for broad level policy change in CVD. EACH published its CV Health Plan for Europe in May 2022 to reduce premature and preventable deaths in the region and improve access to high-quality cardiovascular risk assessment and multidisciplinary care pathways for all, paving the way to a better quality of life.
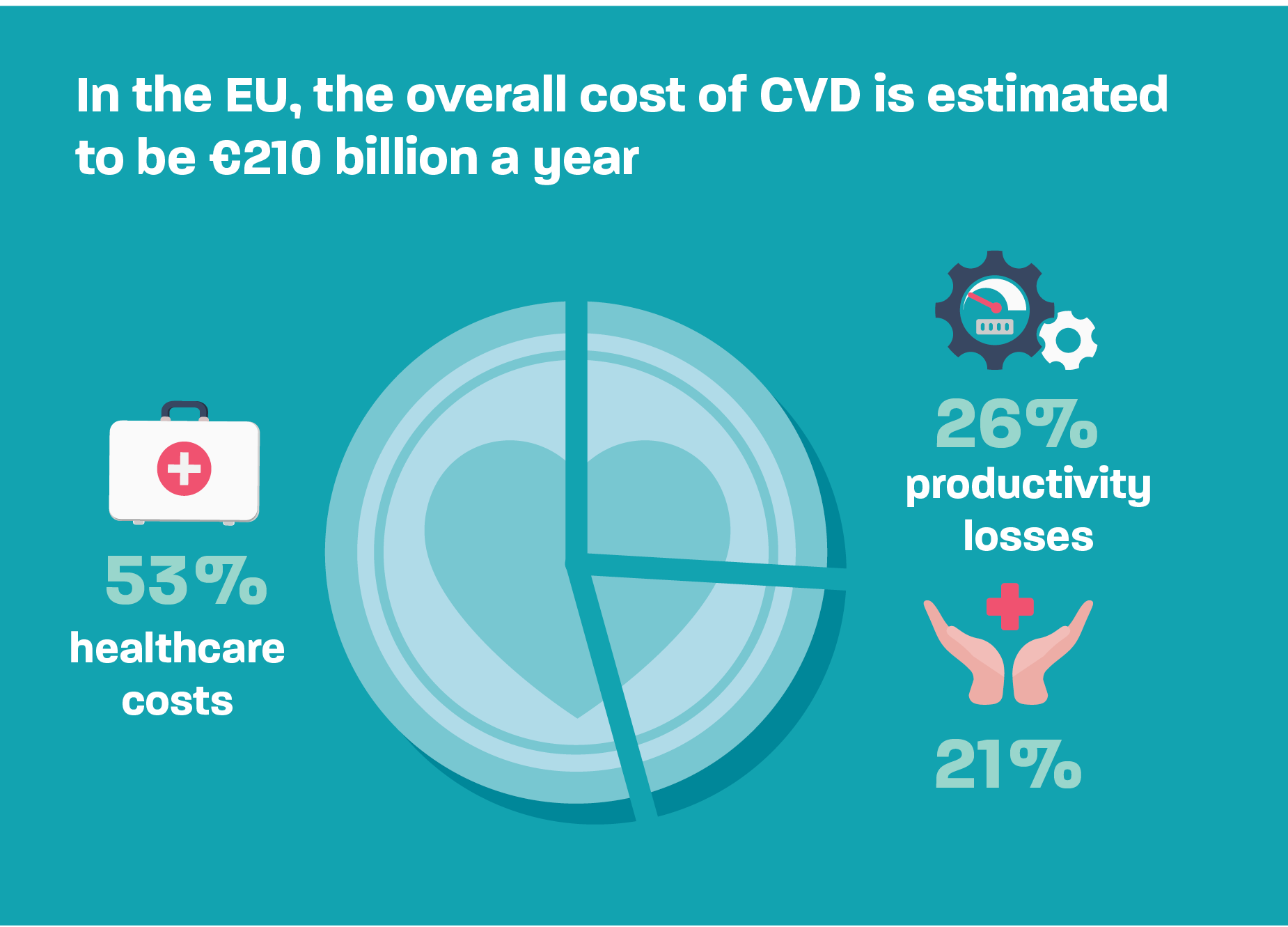
CVD leads to enormous individual, societal and economic challengesIn 2015, the EU economy lost €210 billion to CVD; of which €111 billion (53%) was in health care costs, €54 billion (26%) in productivity losses, and €45 billion (21%) was in the costs of informal care of people with CVD. These costs will increase on a yearly basis driven by the triple threat of demographic changes, lifestyle factors, and climate change.
But also worldwide, CVD is the leading cause of death. In 2019, an estimated 17.9 million people died from CVD, representing 32% of all global deaths. Therefore, the UN Sustainable Development Goals (SDGs) aim to combat NCDs and any newly set up EU strategy should feed into promoting combatting CVD also on a global scale in multilateral and bilateral efforts. EU-CVD-strategies should hence cover both dimensions - the purely EU internal but also EU global health strategy.Thereby, any strategy to reset health care priorities and drive economic stability must address CVDs as a root cause of the stress on our health systems, pressure on our welfare systems, and productivity losses in our workforces. Innovation and digitalization promotion are solutions to creating better health prevention, treatment and coverage for patients. The EU Digital Health Union and EU Innovation initiatives such as IMI, IHI and IPCEI are therefore key also to CVD.
What needs to change? More investments in health care and innovation are necessary to improve outcomes for CVD patients in Europe
Despite the amazing developments in science for CVD patients in the 2nd half of the 20th century, for the first time in 50 years EU countries have reported an increase in premature CVD deaths. As there is continued patient needs in most CVD areas, such as high LDL-C, heart failure, etc, policymakers need to ensure that the right financial and regulatory frameworks are in place to incentivise continued CVD research in Europe and deliver novel treatments to patients to improve and extend their lives.
6 concrete calls to action for policy makers to transform the lives of CVD patients in Europe:


Achieve fast implementation of decisive action to mitigate cardiovascular risk factors through appropriate screening and early detection programmes. This could be done via a yearly heart health check at the primary care level where most of Europe’s CVD-patients are managed. Screening strategies and policies need to be updated to reflect the latest scientific evidence. Healthcare Professionals (HCPs) need to be trained to detect these diseases early to avoid late or misdiagnoses.


Address health inequities across Europe and within countries. Population-wide programmes specifically designed to help countries and regions to overcome these inequities need to be prioritised. Continuous monitoring, specific policies at the EU-level as well as harmonised data registries in the Member States, could help to identify and effectively address inequalities.

Leverage pharmaceutical innovation & collaborative partnerships, including collaboration between public and private entities. This will address the burden of CVD, overcome treatment bottlenecks, and positively influence population health. Pharmaceutical innovation has a role to play in addressing unmet medical needs and seeing improvements in outcomes for CVD patients back on track. This requires strong and stable incentives for innovation in Europe: a state-of-the-art intellectual property framework, a fast and predictable regulatory system and appropriate/holistic valuation of innovation by payers and HTA bodies.
Towards a new normal: Why boosting CV health is critical
The needs around CVD present an opportunity for the EU to demonstrate leadership to achieve the WHO goals, endorsed by the UN, of reducing CVD by 25% by 2025 by promoting the need for comprehensive CVD national action plans, including reduction of mortality targets, establishing targeted screening policies and promoting innovative access schemes and patient identification strategies. For this, innovative thinking and political leadership is needed to change the current inertia and perception that CVD is only a lifestyle driven disease. Additionally, financial and non-financial incentives plus digital solutions for patient identification and risk stratification are needed to support the improved management of CV-conditions.
Boosting cardiovascular health in Europe can provide a key lever for boosting health system resilience and equity. There are three areas to focus on:
- Strengthen population screening
- Ensure treatment initiation, maintenance and follow-up for at-risk patients
- Foster date-driven decision making
Download the report
Improving Secondary Prevention of Cardiovascular Disease in Europe
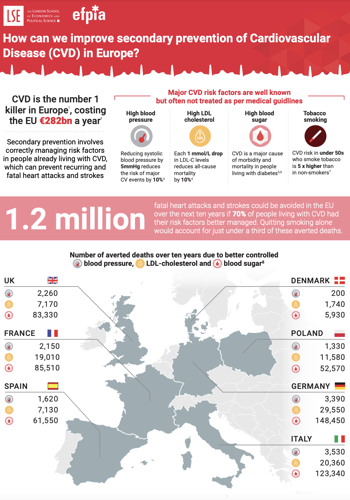
A study by the London School of Economics and Political Science (LSE), commissioned by EFPIA CVH Platform, shows the opportunity of secondary prevention to save hundreds of thousands lives. The report features six recommendations that can reduce the risk of fatal heart attacks and strokes in people living with CVD, by following medical guidelines. Appropriate management of high cholesterol, high blood pressure, high blood glucose and smoking, while encouraging healthier diets and physical activity, can reduce the risk of death from repeat heart attacks and strokes. In fact, the report proposes that more than 1 million fatal CVD events could be avoided in the EU over the next 10 years if 70% of people living with CVD had their risk factors better managed than they are today.
Download the report
Cardiovascular disease (CVD) and unmet medical need (UMN)
Addressing unmet medical need (UMN) is a cornerstone of pharmaceutical innovation as the industry aims to develop treatments that improve and extend peoples’ lives. Taking the patient needs and the evolution of science as a starting point, EFPIA understands an UMN as a condition that is not adequately prevented, treated or diagnosed by authorised interventions. A broad understanding of UMN should recognise and tackle the many ways in which UMNs manifest.
Any definition of UMN that is based on narrow criteria such as disease severity, the presence/absence of current treatment options, or the potential of new treatments to reduce morbidity or mortality can pose great risk to innovation as it disregards the chronic nature of many CVDs and the importance of patient-reported outcomes and experiences.
Find out more
-
Prevention, Use of Health Data and Healthcare Equity: Key Factors for Improving Cardiovascular Health in Spain
Farmaindustria, EFPIA and PwC presented a report titled “Towards a Better Cardiovascular Health in Spain”, which analyses the current situation as well as key areas for improvement.14.06.23Read Article -
How is your country treating your heart? (Guest blog)
A set of CVD data across 22 European countries to see how CVD trends have developed over time, the existing disparities between countries and what key actions can be taken to make a positive difference.12.06.23Read Article -
Boosting health in Europeans: Introducing a cardiovascular & diabetes health check (Guest blog)
Health Checks are an investment in millions of lives26.01.23Read Article -
EFPIA calls for an ambitious EU approach to the challenge of NCDs
EFPIA takes note of the recently announced EU Non-Communicable Diseases (NCDs) Initiative Healthier together by the European Commission, aiming to reduce the burden of NCDs across Europe.03.02.22Read Article -
New industry network committed to address Europe’s number one killer: Cardiovascular related diseases
Improving policy and outcomes for people with cardiovascular related diseases in Europe30.09.21Read Article