Introduction
Introduction:
The power up agenda
It’s time to POWER up health systems
European Union (EU) countries provide some of the best healthcare in the world. Europe has long been a centre of excellence for high-quality healthcare, education, research and innovation. Solidarity is prioritised – with most countries providing universal health coverage for core services.
Nevertheless, the COVID-19 pandemic has pushed health systems to their limits, exposing and exacerbating serious underlying flaws. As well as the enormous direct impact of COVID-19 itself, the pandemic has indirectly caused immense and lasting damage via disruption to routine healthcare services. COVID-19 also amplified pre-existing gaps and variations in disease burden, healthcare access, and outcomes between and within EU countries.
The impact of COVID-19 was exacerbated by health system weaknesses related to decades of under-investment, short-term savings, and misplaced spending on inefficient healthcare models that reward the quantity of care delivered, rather than its quality and the outcomes achieved.
Looking to the future, COVID-19 has propelled health to the top of the political agenda for years to come, and proven how inseparable it is from our prosperity. More than ever before, European citizens rightfully expect strong health systems that meet their needs and those of society at large. The pandemic has also shown the remarkable achievements that are possible when health stakeholders collaborate toward shared goals – for example in delivering innovative technologies and care delivery models.
Now is the time to use the lessons learned from this crisis – positive and negative – and the renewed political and public prioritisation of health, to ambitiously reform our health systems.
Now is the time to ‘POWER up’ our health systems to address the challenges of the 21st century.
Unprecedented challenges warrant ambitious reform
Future health expenditure across the EU, dominated by chronic disease care costs, will continue to grow rapidly unless there is a shift to disease prevention and more sustainable models of care.
At the same time, societal ageing threatens the financing of health with a shrinking working-age fraction of the population having to support rising levels of health spending.
Added to this, health systems face long-term threats from antimicrobial resistance, environmental risks, and climate change.
Ageing challenge in numbers
- By 2100, the proportion of the EU-27 population aged 65 years or over will increase by around 50%, from 20.2% in 2019 to 31.3%.
- The proportion of the very old is growing even faster. For example, the proportion of people aged 80 and over will more than double between 2019 and 2100, from 5.8% to 14.6%.
- The shrinking working age population will have to generate greater tax revenues to support rising societal spending needed to meet the needs of the ageing population. The EU’s old-age dependency ratio is projected to double from 31.4% in 2019 to 57.1% by 2100. This means that by 2100 there would be fewer than two (1.75) persons of working age for every person aged 65 or over, as compared to around three currently.
Chronic disease challenge in numbers
- Almost one third of people aged over 15 years report living with two or more chronic non-communicable diseases (NCDs).
- 37% of Europeans aged 65 and over have multiple chronic conditions, but this figure varies almost three-fold between EU member states.
- Among 10 European countries, the prevalence of multi-morbidity among people aged 50 and above rose from 38% in 2007 to 42% in 2015.
- NCDs account for 9 out of 10 deaths in the EU. Cardiovascular disease and cancers alone account for almost two thirds of deaths in the EU.
- NCDs account for up to 80% of all healthcare spending in the EU. Cardiovascular disease, cancer, type 2 diabetes and chronic respiratory disease alone account for at least 25% of health spending .
- Around 550,000 people of working-age die prematurely every year across the EU due to NCDs, amounting to 3.4 million life-years and €115 billion in economic potential lost annually.
- NCDs also result in hundreds of billions more in informal care, as well as societal costs such as lost production and social welfare.
- Four major NCDs alone result in a 2% loss in gross domestic product across the EU.
- The total health and economic cost of NCDs in the EU is projected to increase by over 70% by 2050.
Inefficiency is holding health systems back, with one in every five Euros spent on health being wasted. Smart spending on pharmaceuticals will be essential to help improve efficiency, but pharmaceuticals account for only one fifth of health expenditure. True efficiency gains will require organisational reform to integrate services and budgets in people-centred ways, and align them toward common goals of improving health outcomes. Only this way can investments in one area generate long-term or system-wide value. Only this way can we secure a sustainable future for our healthcare systems while benefitting patients, healthcare professionals, providers and payers alike.
Health spending is an investment, not a cost
Governments must no longer regard health spending as a cost or burden, or a target for short-term cost-containment, but rather as a societal investment both in the wellbeing of citizens and in our economic future.
Better health drives prosperity. Healthier people enjoy longer and more productive working lives – contributing to the economy while consuming less healthcare.
The health sector is essential to any countries’ economic performance and stability, having a positive impact across other sectors through the jobs it generates and from the purchase of goods and services. It also reduces social exclusion through benefits on employment, working conditions and household income.
The health sector (both public and private) is also in itself a driver of growth and innovation, and one of the largest employers in Europe with a highly skilled workforce.

“The EU should encourage governments to act according to these principles, and to level up health spending across the EU”
Health system spending is therefore a societal investment in our economic future, as well as our health. It builds the foundations for stronger and more sustainable economic growth, which in turn supports better healthcare provision. This ‘virtuous circle’ will help to solve the challenge posed by societal ageing and other long-term threats, and better prepare health systems for future shocks.
This principle already enjoys wide policy support.
- The Tallin Charter of 2008 enshrined the principle of ‘health systems for health and wealth’.
- The ‘economy of wellbeing’ principle, championed by the Finnish Presidency of the EU in 2019, is supported by the Organisation for Economic Co-operation and Development (OECD) and the World Health Organization and the International Monetary Fund also recognise the importance of investing in health.
- Organisations representing over 40 million health professionals from 90 countries have also urged G20 leaders to put health at the centre of their economic recovery packages post-COVID-19.
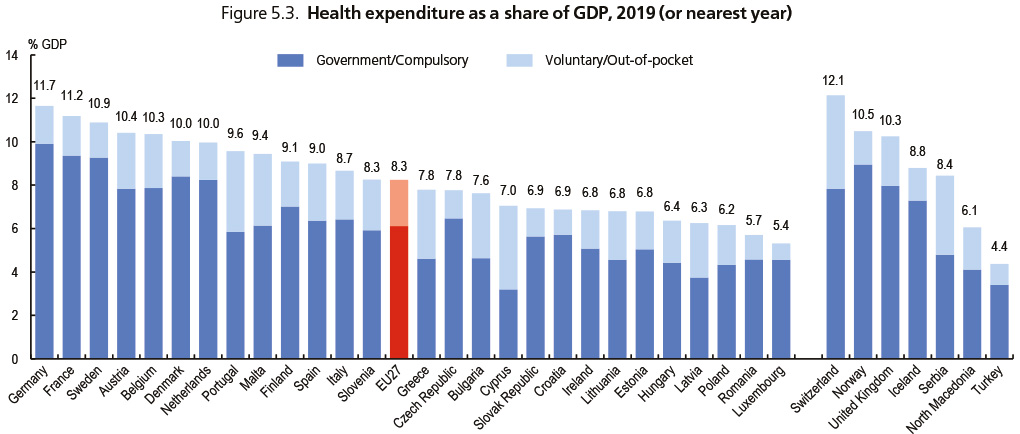
Source: OECD Health Statistics 2020; Eurostat Database; WHO Global Health Expenditure Database.
StatLink: https://stat.link/urm8qw
We and others have advocated and worked for years to modernise health systems according to these principles. So what’s going to make the difference now?
The answer is digitalisation.
Digitalisation is already revolutionising healthcare, but we are only beginning to feel its POWER. Digital health tools proved their worth during COVID-19, providing adaptable new ways for people and health systems to interact. More profoundly, system-wide digitalisation will help unleash the full POWER of data – allowing better and faster decisions to be made throughout our healthcare and innovation systems. In a sense, all healthcare will be digital, with benefits at every level.
Digitalisation is now the difference
Industry – a vital partner in powering up health systems
The European research-based pharmaceutical industry is a vital and committed partner within EU health systems. Research-based companies are critical:
- providers of innovation and technologies that improve and extend patients’ lives and provide efficiency gains for health systems
- pioneers in people-centred, outcomes-based and data-driven healthcare
- partners in intersectoral EU-level and global collaborations, including initiatives to tackle the COVID-19 pandemic and to address longer-term challenges
- as a geostrategic asset for the EU, as a knowledge-based economy, in terms of its research and development, intellectual property production, growth and employment footprint.
However to realise this future, we must POWER up our future health systems. This means investing smartly in five POWER priorities: People-centricity, Outcomes, Workforce empowerment, Efficiency and Resilience. It also means embracing the transformational tools we need – namely digitalisation and innovation that generates value to patients, health systems and society as a whole.
We recognise that national health systems differ in important ways. Nevertheless, we believe that all can and must POWER up to better meet the needs of the citizens they serve, and that these priorities can guide policymakers and healthcare leaders to achieve this transformation.
System-wide change is never easy. However, collaborative actions against COVID-19 have shown what can be achieved when sectors come together towards a common goal.
We cannot afford to fail, and we can only succeed together.
References
Boyce T, Brown C. Economic and social impacts and benefits of health systems. WHO Regional Office for Europe, 2019. Available at https://apps.who.int/iris/handle/10665/329683
Council of the European Union. Council conclusions on the Economy of Wellbeing. (2019/C 400/09), 2019. Available at https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52019XG1126(06)&rid=5
European Parliament Special Committee on Beating Cancer. Public consultation Synopsis Report - The impact of the COVID-19 pandemic on cancer prevention, health services, cancer patients and research: lessons from a public health crisis. European Parliament Special Committee on Beating Cancer, 19 April 2021. Available at https://www.europarl.europa.eu/cmsdata/232900/Synopsis%20report%20BECA%20COVID-19%20Consultation%20.pdf
Eurostat. Population structure and ageing. 2020. Available at https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing#The_share_of_elderly_people_continues_to_increase
In support of a #HealthyRecovery https://healthyrecovery.net
International Monetary Fund. A strategy for IMF engagement on social spending. 2019. Available at https://www.imf.org/en/Publications/Policy-Papers/Issues/2019/06/10/A-Strategy-for-IMF-Engagement-on-Social-Spending-46975
IQVIA. EFPIA Patients wait indicator survey. 2020. Available at https://www.efpia.eu/media/554526/patients-wait-indicator-2019.pdf
Jagric T, et al. The impact of the health-care sector on national economies in selected European countries. Health Policy 2021;125:90–7
Jansen C, Amesz B. Every day counts – the impact of COVID-19 on patient access to cancer care in Europe. EFPIA, 2021. Available at https://efpia.eu/media/602636/every-day-counts-covid19-addendum.pdf
Kyriakides S. Keynote speech by Commissioner Kyriakides Value-based healthcare conference’, 4 March 2021. Available at https://ec.europa.eu/commission/commissioners/2019-2024/kyriakides/announcements/keynote-speech-commissioner-kyriakides-value-based-healthcare-conference_en
Masters R, et al. Return on investment of public health interventions: a systematic review. J Epidemiol Community Health 2017;71:827–34
Nozal AL, et al. The economy of well-being: creating opportunities for people’s well-being and economic growth. OECD, 2019. Available at https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=SDD/DOC(2019)2&docLanguage=En
OECD. Health at a glance 2019: OECD indicators. OECD, 2019. Available at https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2019_4dd50c09-en
OECD/European Union. Health at a Glance: Europe 2020: State of Health in the EU Cycle. OECD, 2020. Available at https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-europe-2020_82129230-en?_ga=2.52510440.1357533625.1626362665-1150508910.1626362665
OECD. Tackling wasteful spending on health. 2017. Available at https://www.oecd.org/health/tackling-wasteful-spending-on-health-9789264266414-en.htm
OECD. The economy of wellbeing – creating opportunities for people’s well-being and economic growth, 2019. Available at https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=SDD/DOC(2019)2&docLanguage=En
Palladino R, et al. Multimorbidity and health outcomes In older adults In ten European health systems, 2006–15. Health Affairs 2019;38:613–23
Palm W, et al. Gaps in coverage and access in the European union. Health Policy 2021;125:341–50
Rechel B, Jagger C, McKee M. The Economics of healthy and active ageing. European Observatory on Health Systems and Policies / WHO, 2020. Available at https://eurohealthobservatory.who.int/publications/i/living-longer-but-in-better-or-worse-health
Tallinn Charter. Health systems for health and wealth. WHO European Ministerial Conference on Health Systems, Tallinn, Estonia; 27 June 2008. Available at https://www.euro.who.int/__data/assets/pdf_file/0008/88613/E91438.pdf
United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430). 2019. Available at https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf
Vandenberghe D, Albrecht J. The cost of non-communicable diseases in the European Union; A future projection. Proceedings of International Academic Conferences 9412102, International Institute of Social and Economic Sciences, 2019. Available at https://ideas.repec.org/p/sek/iacpro/9412102.html
Vandenberghe D, Albrecht J. The financial burden of non-communicable diseases in the European Union: a systematic review. Eur J Public Health 2020;30:833–9
Williams G, Cylus J, Roubal T, et al. Sustainable health financing with an ageing population: Will population ageing lead to uncontrolled health expenditure growth? WHO/European Observatory on Health Systems and Policies, 2020. Available at https://apps.who.int/iris/bitstream/handle/10665/329382/Policy-brief-1997-8073-2019-3-eng.pdf
World Bank. Cause of death, by non-communicable diseases (% of total) – European Union, 2019. Available at https://data.worldbank.org/indicator/SH.DTH.NCOM.ZS
World Bank group. Health. Available at https://www.worldbank.org/en/topic/health/overview
WHO Regional Office for Europe. European programme of work 2020–2025. 2020. Available at https://apps.who.int/iris/bitstream/handle/10665/339209/WHO-EURO-2021-1919-41670-56993-eng.pdf?sequence=1&isAllowed=y
WHO Regional Office for Europe. Health inequity and the effects of COVID 19: assessing, responding to and mitigating the socioeconomic impact on health to build a better future. 2020. Available at https://apps.who.int/iris/bitstream/handle/10665/338199/WHO-EURO-2020-1744-41495-56594-eng.pdf