Outcomes
matter most
Outcomes
matter most
Future health systems should focus on delivering and paying for what matters most – better health and longer lives.
People at heart, outcomes in mindCurrent healthcare systems tend to focus on the amount of healthcare delivered, not the value it actually brings to patients, health systems and society.
For example, healthcare funders mostly measure and pay for healthcare according to the number of tests, services, procedures and medicines provided. Inevitably, resources are focused on meeting these targets rather than on delivering the health outcomes that matter most to patients and society.
This can lead to:
- poor efficiency – by incentivising the overuse of inappropriate healthcare
- underprovision of care or cherry-picking of patients with lesser care needs – especially for simple capitation models where providers are remunerated on the basis of a fixed number of registered patients regardless of how much care they need
- under-investment in interventions and activities that will improve outcomes in the long term.
This is not relevant only to certain services, therapy areas, patient groups and medicines: it should apply as an organisational principle across the whole health system.
Focusing on outcomes allows health systems to be more:
- people-centric: through the complementary use of patient-reported outcomes and clinical outcomes (see panel). Clinical outcomes (such as blood-sugar levels, tumour growth and mortality) are important but do not give the full picture of the end result of care. Patient-reported outcomes (such as quality of life, psychological wellbeing and physical functioning) allow patients to communicate and engage better with health systems and care to be assessed according to outcomes that matter most to patients themselves. Making aggregate outcomes data publicly available also helps patients make better-informed choices about the healthcare they receive
- integrated: because different services are incentivised to work together toward the same ultimate aim – to measurably achieve the best result for patients
- efficient: by allowing resources to be allocated toward achieving the best health outcomes relative to cost (i.e. from low-value to high-value care) and potentially to realise savings elsewhere or in the longer term; this in turn can improve sustainability
- quality-driven: by creating digital ‘learning systems’ that systematically, consistently and continuously measure standardised outcomes – helping physicians and health services to get real-time feedback on the quality of care and benchmark their performance against their peers and to rapidly share best practices, provided there is transparent reporting
- equitable: by identifying and thereby helping to overcome the existing unwarranted variations in outcomes within and between providers, regions and countries
- innovative: by incentivising investment in innovations in service delivery and technologies that generate better value.
What are outcomes?
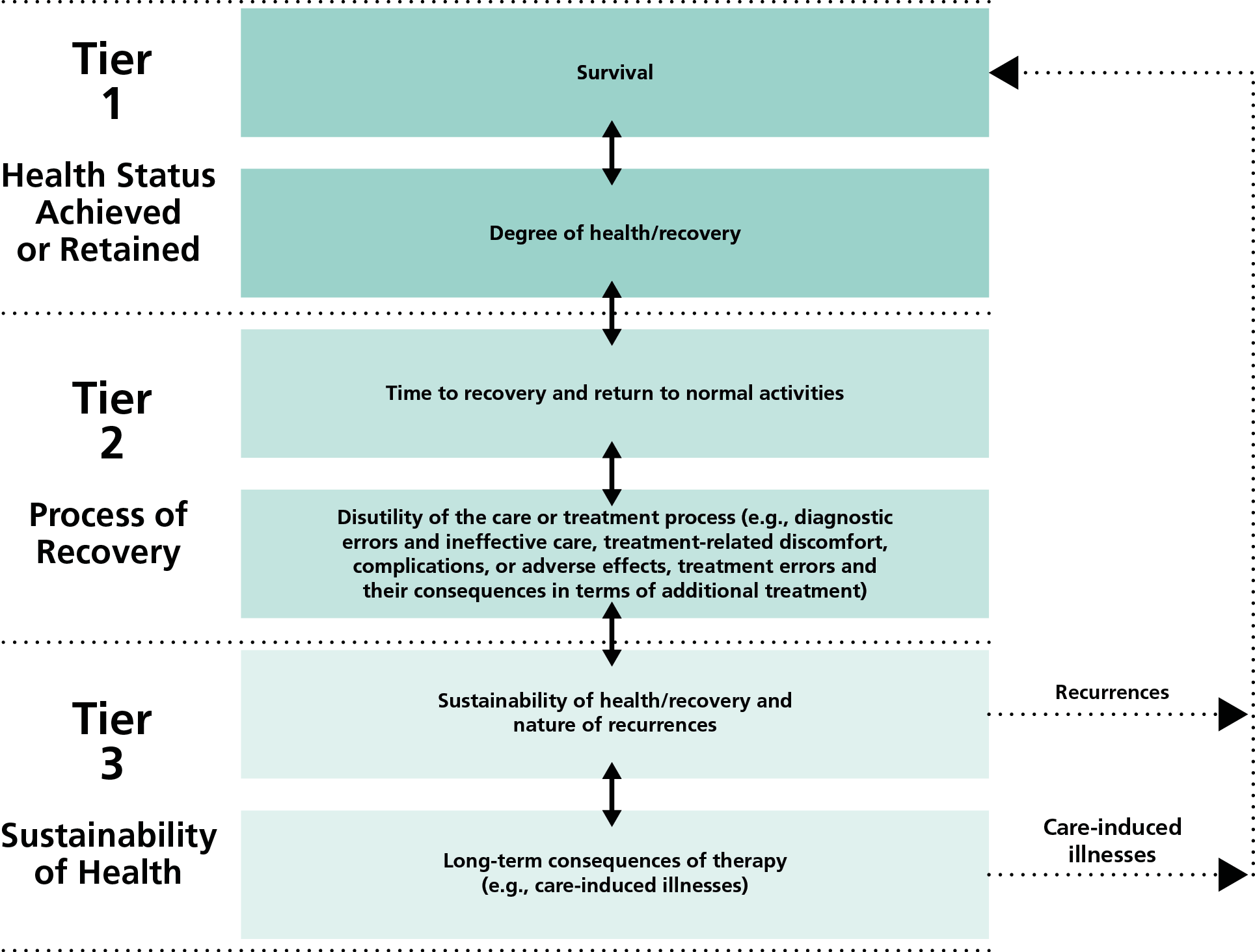
Porter defined outcomes as ‘the results of care in terms of patients’ health over time’. Outcomes are distinct from care processes or interventions, and from biological indicators that merely predict results.
Key principles of outcomes measurement include:
- Outcomes should involve the health circumstances most relevant to patients.
- Outcomes should cover both near-term and longer-term patient health to encompass the ultimate results of care. This includes the full cycle of care, including acute care, related complications, rehabilitation, and reoccurrences.
- Outcomes should cover the full range of services (and providers) that jointly determine the patient’s results.
Each medical condition (or population of primary care patients) will have its own unique set of outcome measures. However, Porter defined the following general hierarchy for outcomes (reproduced with permission from Porter 2010).
The transition to outcomes-based healthcare will include several key steps.
Defining standardised and people-centred outcomes
Health systems should measure standardised outcomes metrics to allow comparison between healthcare providers, regions and even countries. This will allow benchmarking, identification of unwarranted variation, and the sharing of best and worst practices to improve patient outcomes, care quality and value, leading to more informed patients’ choices and better health.
These outcomes are best defined through a multidisciplinary approach with a strong patient involvement. Important initiatives include the International Consortium for Health Outcomes Measurement (ICHOM), the OECD Patient-reported Indicator Surveys (PaRIS) and the Health Outcomes Observatory project.
Transitioning to outcomes-based systems: step-by-step
Measuring outcomes: harnessing digital power
EU health systems need integrated, interoperable digital systems to collect and integrate high-quality outcomes data from many sources under clear governance (See Digital-Health).
Transparent reporting of outcomes data, following the model of countries like Sweden, is also important to allow benchmarking of health outcomes within and across countries, and to inform decision-making by policymakers, service providers, payers and patients.
Paying for outcomes – incentivisation through new models
The transition to outcomes-based healthcare is held back not by technical barriers, but by organisational and cultural barriers, including a lack of incentives. Health systems do not systematically incentivise healthcare providers to measure or report outcomes.
To unblock this, future financing and payment models should shift toward rewarding health outcomes, for example learning from:
- bundled payments that include the provision of rehabilitation and any necessary reoperation after surgery, which incentivise high-quality care
- funding of integrated care models through shared savings contracts
- introduction of pay-for-performance schemes in primary care
- value-based reimbursement agreements for innovative medicines (See Innovation).
These models have yet to be applied at scale across integrated health systems, and there is no one-size-fits-all approach that works for all types of providers, services and products. More work is therefore required to agree on the outcomes to be measured, how to design fit-for-purpose contractual models and the way in which to implement the necessary data collection systems and how best to overcome legal, logistical and administrative barriers.
When used for the purpose of payment models, it is also important that outcomes measures are ‘risk-adjusted’ to account for factors that may affect health outcomes besides the intervention or service to be reimbursed, including patient characteristics (such as age and comorbidities) and whether the treatment was administered properly.
The industry is committed to maximizing the value that our innovations bring to patients, health systems and society and strongly support a transition to outcomes-based care.
We believe in empowering people to have control over their care, outcomes and health data – and we are taking a lead by investing and collaborating with patients, professionals and other health systems partners toward this end.
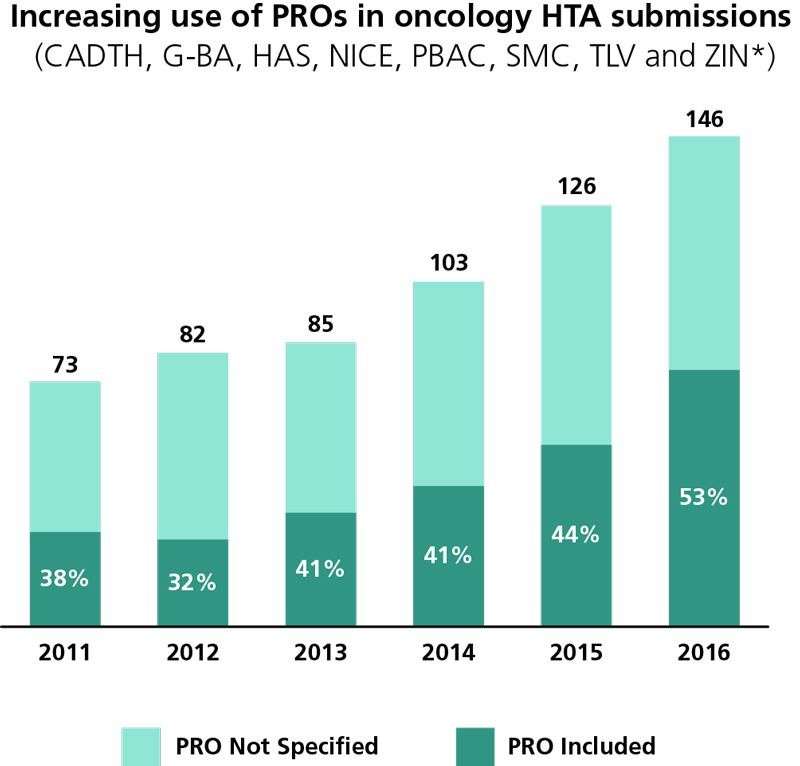
The industry is increasingly incorporating patient-reported outcomes in clinical trials and in regulatory and HTA submissions.
- Between 2012 and 2016, 70% of oncology indications for 49 medicines approved by the European Medicines Agency and Food and Drugs Administration included PRO data in their regulatory submissions.
- In 2016, just over half of HTA submissions made to eight agencies included PROs.
The industry is also engaged in several public-private partnerships to support the use of PROs in healthcare decision-making, including through the Innovative Medicines Initiative.
H2O will allow patients to measure their outcomes in a standardised way, whilst keeping full control of their data. It will enable ethical, secure analysis of the data when patients consent to this, in the interest of society, science and patient care. Ultimately, it aims to foster innovation in healthcare across Europe and beyond to deliver better outcomes for all.
Other relevant projects include the European Health Data and Evidence Network (EHDEN; See Digital-Health), HARMONY, ROADMAP, BigData@Heart and PIONEER.
Case studies
Combining new tools in Danish healthcare to drive value by delivering better patient outcomes
References
EFPIA. Healthier future. The case for outcomes-based sustainable healthcare. 2020.
Available at https://www.efpia.eu/media/412313/the-case-for-outcomes-document-17102018.pdf
EFPIA. Addressing healthcare challenges. Novel pricing and payment models: new solutions to improve patient access. 2020. Available at https://efpia.eu/media/554543/novel-pricing-and-payment-models-new-solutions-to-improve-patient-access-300630.pdf
EFPIA. Strengthening health systems through smart spending. 2020 https://www.efpia.eu/news-events/the-efpia-view/statements-press-releases/strengthening-health-systems-through-smart-spending/
IQVIA. EFPIA pipeline review 2021 update. Available at https://www.efpia.eu/media/602563/iqvia_efpia_pipeline-review_final.pdf
OECD. Better ways to pay for healthcare. OECD, 2016
https://www.oecd.org/publications/better-ways-to-pay-for-health-care-9789264258211-en.htm
Porter ME. What is value in health care? N Engl J Med 2010;363:2477–81
Smith PC, et al. Building on value-based healthcare. Towards a health system perspective. European Observatory on Health Systems and Policies, 2020 https://eurohealthobservatory.who.int/publications/i/building-on-value-based-health-care-towards-a-health-system-perspective-2020-brief
The value of health: improving outcomes – final report. 2016.
Available at https://www.europeanallianceforvalueinhealth.eu/wp-content/uploads/2020/11/The-Value-of-Health-Improving-Outcomes.pdf
Porter ME. Measuring Health Outcomes: The Outcome Hierarchy, Supplementary Appendix 2 to Porter ME. What is value in health care? N Engl J Med 2010;363:2477–81. Available at: https://ichom.org/files/articles/nejmp1011024_appendix2.pdf